Navigating the immense pressures of modern healthcare often forces hospital administrators into a constant cycle of reaction, putting out fires as they arise rather than preventing them. This perpetual state of crisis management stretches resources thin, impacts staff morale, and can ultimately compromise patient care. In an effort to break this cycle, researchers, in collaboration with regional National Health Service (NHS) bodies, have pioneered an operational AI forecasting model engineered to transform how healthcare systems anticipate and meet public demand. This innovative tool moves beyond the common applications of AI in individual diagnostics, instead offering a panoramic view of the entire healthcare ecosystem. By analyzing years of historical public sector data, the model provides leaders with the foresight to make strategic, forward-looking decisions about staffing, resource allocation, and infrastructure, heralding a significant shift from reactive problem-solving to proactive, data-informed planning. This system-level intelligence aims to create a more resilient, efficient, and responsive healthcare service capable of weathering the demographic and epidemiological shifts of the coming years.
A New Paradigm in Healthcare Management
From Reactive Fixes to Proactive Strategies
The traditional model of healthcare management frequently operates on a short-term basis, responding to immediate needs and sudden surges in patient volume. This approach, while necessary in emergencies, lacks the strategic depth required for long-term sustainability and efficiency. The newly developed AI model fundamentally alters this dynamic by empowering healthcare leadership to adopt a proactive posture. It achieves this by generating detailed short-, medium-, and long-term forecasts that predict shifts in healthcare demand with remarkable accuracy. This allows managers to conduct “do nothing” assessments, a powerful feature that quantifies the future consequences of maintaining the status quo. By modeling the cascading effects of inaction—such as increased wait times, bed shortages, or staff burnout—the tool provides a compelling, data-backed case for preemptive intervention. This foresight is invaluable for justifying investments in new staff, expanded facilities, or preventative community health programs before a crisis emerges, ensuring resources are allocated where they will have the greatest impact.
This strategic modeling capability extends beyond simple resource management to directly influence patient outcomes, particularly for the growing demographic of individuals with chronic conditions. A healthcare system that can accurately predict a rise in diabetes-related hospitalizations or an increased need for cardiac care in a specific region can proactively bolster its specialized services. This might involve hiring more endocrinologists, expanding cardiac rehabilitation facilities, or launching targeted public health campaigns aimed at prevention. By anticipating these needs, the NHS can ensure that patients receive timely and appropriate care, reducing the likelihood of emergency admissions and improving long-term health. This shift from a generalized, reactive system to a tailored, predictive one ensures that care pathways are optimized for the specific demographic and health profiles of the population being served. It represents a move toward a more intelligent and compassionate form of healthcare delivery, where data is leveraged not just to treat illness but to anticipate and mitigate it.
The Power of System-Wide Forecasting
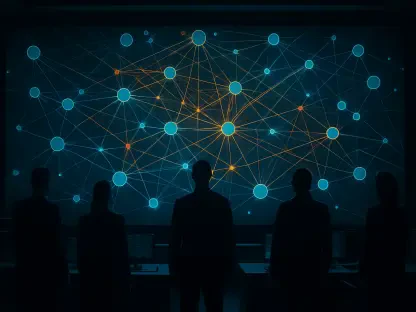
While artificial intelligence in medicine often makes headlines for its role in diagnosing diseases from scans or personalizing treatment plans, this project takes a deliberately different approach. Its focus is not on the individual patient but on the operational health of the entire system. This macro-level perspective provides a crucial tool for leaders tasked with managing the complex interplay of hospitals, community clinics, and long-term care facilities. The model offers a holistic view, analyzing how pressures in one area—such as a shortage of primary care physicians—might create bottlenecks and increased demand in another, like hospital emergency rooms. By understanding these system-wide dynamics, administrators can make more informed decisions about infrastructure development, workforce planning, and service integration. This system-level intelligence allows for the optimization of the entire patient journey, ensuring smoother transitions between different levels of care and a more efficient use of the collective resources available across a region.
This departure from clinical AI toward operational AI addresses a critical gap in healthcare management. It provides a common operational picture for diverse stakeholders, from hospital executives to public health officials, enabling coordinated and cohesive planning. For instance, the model can simulate the impact of closing a specific ward or opening a new community health hub, allowing leaders to assess the potential benefits and drawbacks before committing significant resources. This ability to model various scenarios provides an unprecedented level of strategic agility. It transforms planning from an exercise based on historical trends and educated guesses into a dynamic, data-driven process. The ultimate goal is to create a healthcare ecosystem that functions not as a collection of siloed entities but as an integrated network, with each component optimized to support the others, ensuring resilience and responsiveness in the face of fluctuating patient demand and evolving public health challenges.
The Data-Driven Foundation and Future Trajectory
Integrating Diverse Data for Granular Predictions
The predictive power of this AI model is derived from its ability to synthesize a vast and diverse array of data sources. The system builds its projections by analyzing five years of comprehensive historical records, creating a rich foundation for understanding past trends and future probabilities. This dataset includes a wide range of crucial metrics, such as hospital admission rates, specific treatments administered, patient re-admissions, and fluctuating bed capacity levels. Furthermore, it integrates workforce data, accounting for staff availability and potential shortages, alongside metrics on infrastructure pressures that could impact service delivery. This multifaceted approach ensures that the model’s forecasts are not based on a single variable but on the complex, interconnected web of factors that define the operational reality of the healthcare system. By learning from this deep historical context, the AI can identify subtle patterns and correlations that would be nearly impossible for human analysts to detect.
A key element that elevates the model’s accuracy beyond generic forecasting is its incorporation of detailed local demographic factors. The system doesn’t just look at what happened; it considers who it happened to. By integrating data on age, gender, ethnicity, and, critically, local deprivation levels, the model creates far more nuanced and context-aware predictions. It understands that healthcare needs are not uniform and that a community’s unique demographic profile is a primary driver of demand. For example, an aging population will have different healthcare requirements than a younger one, and areas with higher levels of deprivation often experience a greater burden of chronic disease. By weaving this granular demographic information into its analytical framework, the AI can tailor its forecasts to the specific needs of the communities being served, allowing for more precise and equitable resource allocation that truly reflects the on-the-ground reality.
Scaling for Impact and Enhancing Precision
The project’s initial success was cultivated within a focused testing environment, allowing for refinement and validation in active hospital settings. This phase proved the model’s viability and laid the groundwork for a more ambitious and impactful deployment. The development roadmap, established by the University of Hertfordshire Integrated Care System partnership, always envisioned a broader application, with a planned expansion designed to bring this predictive power to community services and care homes. This step was crucial, as it recognized that modern healthcare is an interconnected ecosystem where pressures and demands flow seamlessly between acute hospital settings and community-based care. By extending the model’s reach, planners could gain a more complete picture of the patient journey and allocate resources more effectively across the entire continuum of care, from preventative services to long-term support.
A significant leap forward in the project’s evolution was realized with the merger of several regional health boards into the new Central East Integrated Care Board. This consolidation brought a population of 1.6 million residents under a single administrative umbrella, creating an unprecedented opportunity to scale the AI model’s capabilities. The integration of data from this much larger and more diverse population was expected to dramatically improve the model’s predictive accuracy and utility. A larger dataset provides more examples for the AI to learn from, allowing it to identify more subtle trends and make more reliable forecasts. This expansion marked a pivotal moment, transforming the initiative from a promising pilot into a robust, large-scale operational tool with the potential to fundamentally reshape healthcare planning for a vast segment of the population. The enhanced precision achieved through this expansion promised a future of more resilient and responsive public health management.