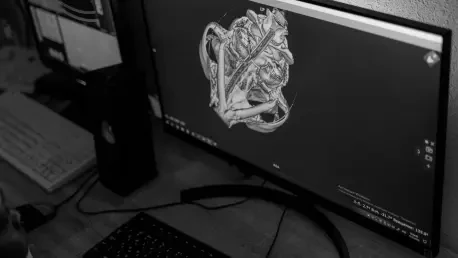
In the intricate world of pediatric radiology, obtaining high-quality magnetic resonance imaging (MRI) for children poses significant challenges due to factors like motion artifacts, inherent noise, and the necessity for prolonged scan durations that can distress young patients. A pioneering study published in Pediatric Radiology has unveiled a transformative approach by harnessing deep learning, an advanced facet of artificial intelligence (AI), to elevate the quality of pediatric abdominal MRI. This research, conducted by Zucker, Milshteyn, Machado-Rivas, and colleagues, focuses on refining images captured through 3D T1 fast spoiled gradient echo (FGRE) acquisitions. By integrating AI-driven reconstruction techniques, the study not only tackles longstanding imaging hurdles but also promises to enhance diagnostic precision and improve the overall experience for children undergoing these critical procedures. This article explores the innovative application of deep learning, its impact on clinical outcomes, and the broader implications for pediatric healthcare.
Transforming Imaging Challenges with AI
The core of this groundbreaking research lies in addressing the persistent difficulties associated with pediatric abdominal MRI, where traditional methods like 3D T1 FGRE, while effective in providing detailed anatomical views, often falter due to children’s natural tendency to move during scans. Such movements result in motion artifacts that blur images, compounded by inherent noise that can mask crucial diagnostic details. These issues not only hinder the ability to identify conditions such as tumors or cysts but also place emotional and physical strain on young patients who struggle to remain still for extended periods. The introduction of deep learning offers a promising solution by employing sophisticated algorithms trained on extensive datasets of pediatric MRI scans. These algorithms are designed to detect and correct distortions, paving the way for images of unprecedented clarity that can significantly aid in accurate diagnosis.
Beyond merely correcting visual imperfections, the AI-driven approach brings an additional advantage by substantially reducing scan times, a critical factor in pediatric imaging. Shorter durations mean less time for children to endure the confines of an MRI machine, thereby alleviating anxiety and discomfort for both the patients and their families. This efficiency does not come at the cost of quality; instead, the deep learning model enhances the resolution of images, ensuring that radiologists have access to reliable data for their assessments. The dual impact of improved visuals and quicker procedures marks a significant shift in how pediatric MRI is conducted, addressing two major pain points simultaneously. As a result, this technology sets a new benchmark for patient-centered care in radiology, prioritizing both diagnostic accuracy and emotional well-being.
Elevating Diagnostic Precision and Workflow Efficiency
One of the most profound benefits of integrating deep learning into pediatric abdominal MRI is the marked improvement in diagnostic accuracy that clearer images provide. With reduced noise and artifacts, clinicians can identify subtle abnormalities with greater confidence, a factor that is especially vital in pediatric care where early detection can dramatically influence treatment outcomes. The study substantiates these advancements through objective metrics such as signal-to-noise and contrast-to-noise ratios, offering tangible evidence of the algorithm’s effectiveness. This heightened precision empowers medical professionals to initiate timely interventions, potentially altering the course of serious conditions and enhancing long-term health prospects for young patients who rely on accurate diagnoses for effective care plans.
Additionally, the incorporation of AI into the diagnostic process streamlines clinical workflows, creating a more efficient environment for radiologists. By automating the enhancement of MRI images, the deep learning model eliminates the need for labor-intensive manual adjustments, freeing up valuable time for specialists to focus on intricate case evaluations and direct patient interactions. This synergy between advanced technology and human expertise optimizes the balance of routine tasks and complex decision-making, fostering a healthcare system that is both responsive and tailored to the unique needs of children. The efficiency gained through this approach not only benefits individual practitioners but also has the potential to improve overall hospital operations, ensuring that more patients receive prompt attention without compromising the quality of care delivered.
Navigating Ethical and Practical Considerations
While the advantages of deep learning in pediatric MRI are compelling, the research also brings to light several challenges and ethical considerations that must be addressed to ensure responsible implementation. Key among these are concerns surrounding data privacy, as the algorithms rely on vast amounts of patient information for training, raising questions about how such sensitive data is safeguarded. Furthermore, there is the risk of biases embedded within the training datasets that could skew results, potentially leading to disparities in diagnostic accuracy across diverse patient groups. These issues necessitate stringent protocols to protect confidentiality and ensure fairness, highlighting the importance of transparency in the development and deployment of AI tools within medical settings.
Equally significant is the caution against over-reliance on technology, which could undermine the critical role of human judgment in radiology. The study emphasizes that AI should serve as a complementary tool rather than a substitute for clinical expertise, advocating for a balanced approach where technology enhances rather than dictates decision-making processes. This perspective aligns with a broader trend in healthcare that seeks to harmonize innovation with ethical responsibility, ensuring that advancements like deep learning in pediatric imaging prioritize patient safety and equity. By fostering rigorous oversight and continuous validation, the medical community can harness the full potential of AI while mitigating risks, creating a framework that supports sustainable progress in pediatric radiology for years to come.
Future Horizons in Pediatric Radiology
Reflecting on the strides made by this research, it becomes evident that deep learning reconstruction techniques have already redefined standards in pediatric abdominal MRI by tackling issues of noise, artifacts, and lengthy scan times with remarkable success. The improvements in image quality and procedural efficiency achieved through this study have directly translated into better diagnostic outcomes and reduced stress for young patients and their families. These advancements, driven by the collaborative efforts of researchers and clinicians, have laid a robust foundation for enhancing pediatric care through technology, demonstrating the tangible benefits of AI in a clinical context.
Looking ahead, the next steps involve expanding the application of these AI-driven techniques to other areas of medical imaging and diverse patient populations, building on the success seen in abdominal MRI. Continued research should focus on refining algorithms to address even more complex imaging challenges while developing comprehensive ethical guidelines to govern AI use in healthcare. Encouraging partnerships between technologists and medical professionals will be crucial in driving innovation, ensuring that future developments remain aligned with the goal of improving patient-centered care. As the field progresses, the integration of deep learning promises to unlock new possibilities, shaping a future where precision and compassion converge to support the health and well-being of children worldwide.