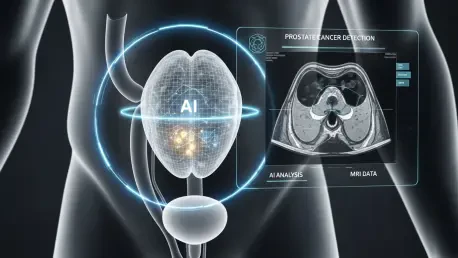
In a world where prostate cancer remains one of the leading health threats to men globally, a transformative breakthrough in medical imaging has emerged to redefine the battle against this disease, with millions of new cases diagnosed each year. The challenge of accurate and timely detection has long plagued healthcare systems, often resulting in delayed treatments or unnecessary interventions due to inconsistent diagnostic methods. Enter an innovative AI-powered MRI system, a cutting-edge tool that harnesses the capabilities of artificial intelligence to enhance the precision of prostate cancer detection. Developed through extensive research and rigorous clinical validation, this technology promises not only to improve diagnostic accuracy but also to address systemic inequities in healthcare access. By integrating deep learning algorithms, specifically convolutional neural networks (CNNs), this system offers a standardized approach to interpreting complex MRI scans, potentially saving countless lives through earlier and more reliable diagnoses.
Harnessing AI for Breakthrough Imaging
This AI-driven MRI system represents a monumental leap in medical technology, leveraging sophisticated deep learning models to analyze multiparametric MRI scans with unprecedented detail. Trained on vast datasets of imaging paired with confirmed biopsy outcomes, the system excels at identifying subtle indicators of clinically significant prostate cancer that might be overlooked by human eyes. Unlike traditional methods where interpretation can vary widely based on a radiologist’s experience, this technology provides a consistent framework for diagnosis. The use of convolutional neural networks allows the tool to detect intricate patterns in imaging data, distinguishing aggressive tumors from benign conditions with remarkable accuracy. Such a capability not only elevates the standard of care but also reduces the burden on specialists by offering a reliable second opinion, ensuring that critical cases are prioritized for further evaluation and intervention.
The impact of this technological advancement extends beyond mere detection to fundamentally altering how medical imaging is perceived in clinical settings. By minimizing subjectivity, the system helps standardize diagnostic outcomes across different facilities, whether in urban hospitals or rural clinics. This consistency is vital for building trust among patients and healthcare providers, as it ensures that a diagnosis is based on objective data rather than varying human judgment. Furthermore, the reduction in false positives translates to fewer unnecessary biopsies, sparing patients from invasive procedures and the associated anxiety. As a result, resources can be allocated more effectively, focusing on those who truly need urgent care. This AI-powered approach marks a pivotal shift toward precision medicine, where technology and human expertise collaborate to deliver better health outcomes on a broader scale.
Elevating Diagnostic Precision
One of the most compelling strengths of this AI-enhanced MRI system lies in its ability to achieve diagnostic precision that rivals or surpasses that of seasoned radiologists. Through extensive validation studies involving diverse patient populations and a variety of scanning equipment, the technology has demonstrated exceptional sensitivity and specificity in identifying significant prostate cancer. This reliability holds steady regardless of differences in imaging protocols or demographic factors, addressing a critical gap in traditional screening methods where inconsistency often leads to missed diagnoses or over-treatment. Such robust performance offers a lifeline to patients by ensuring that life-threatening conditions are caught early, paving the way for timely and appropriate medical responses that can dramatically improve survival rates.
Equally significant is the system’s role in reducing diagnostic variability, a persistent issue in prostate cancer screening that can result in unequal care. By providing a uniform standard of analysis, the technology ensures that a patient’s outcome does not hinge on the subjective interpretation of a single practitioner or the quality of equipment at a specific location. This standardization is particularly crucial in preventing overdiagnosis, which can lead to unnecessary stress and medical costs for patients facing benign or low-risk conditions. With the AI system acting as a consistent benchmark, healthcare providers can make more informed decisions, tailoring interventions to the actual severity of the disease. This approach not only enhances trust in diagnostic processes but also streamlines the path from detection to treatment, ensuring that resources are directed where they are most needed.
Optimizing Clinical Efficiency
Beyond its diagnostic prowess, the AI-powered MRI system is engineered for seamless integration into the fast-paced environment of clinical practice, making it a practical asset for healthcare professionals. It produces intuitive outputs such as heatmaps and lesion segmentations overlaid on MRI images, offering clear visual cues that simplify complex data for radiologists. These tools facilitate effective communication during multidisciplinary team discussions and patient consultations, ensuring that critical information is easily understood and acted upon. By bridging the gap between intricate AI algorithms and everyday medical decision-making, the system enhances collaboration among specialists, ultimately improving the quality of care delivered to patients in diverse settings.
Another key advantage is the system’s rapid processing capability, which significantly boosts efficiency in overburdened radiology departments. In many healthcare facilities, delays in imaging analysis can hinder timely diagnosis and treatment, creating bottlenecks that affect patient throughput. This technology addresses that challenge by delivering results at an accelerated pace without compromising accuracy, allowing more individuals to be screened in less time. Such efficiency is invaluable for high-volume centers and under-resourced clinics alike, where the demand for diagnostic services often outstrips capacity. By alleviating these pressures, the system ensures that advanced prostate cancer screening becomes a feasible component of routine care, enhancing overall access to life-saving interventions.
Navigating Ethical and Privacy Challenges
As transformative as this AI technology is, its deployment comes with a responsibility to address ethical and privacy concerns that are paramount in healthcare innovation. Developers have prioritized transparency and accountability by incorporating frameworks like federated learning, which allows the system to evolve and improve without jeopardizing patient data confidentiality. This method ensures that sensitive information remains secure while still enabling the model to adapt to new clinical insights and imaging advancements. Compliance with stringent regulatory standards further reinforces the commitment to responsible implementation, fostering confidence among medical professionals and patients who rely on the integrity of such tools for critical health decisions.
Moreover, the system is deliberately positioned as an assistive resource rather than an autonomous decision-maker, preserving the essential role of human judgment in medicine. Radiologists remain at the forefront of the diagnostic process, using the AI’s insights to enhance their expertise rather than replace it. This balance ensures that technology serves as a partner, augmenting clinical skills while maintaining the personal connection that defines patient care. By emphasizing ethical deployment, the system upholds the trust necessary for widespread adoption, ensuring that advancements in AI contribute positively to healthcare without overstepping boundaries of privacy or professional oversight. This careful approach sets a precedent for future innovations in medical technology.
Promoting Global Health Equity
Among the most profound implications of this AI-powered MRI system is its potential to bridge disparities in prostate cancer care, particularly in regions where access to specialized expertise is limited. In many underserved areas, the scarcity of trained radiologists can delay or prevent accurate diagnoses, leading to higher mortality rates from treatable conditions. This technology offers a solution by providing high-fidelity diagnostic support, enabling earlier detection even in settings with minimal resources. Such accessibility can be a game-changer for communities that have historically been left behind in the advancement of medical care, offering a chance to reduce preventable deaths through timely intervention.
The system’s design also prioritizes scalability and cost-effectiveness, making it a viable option for implementation in resource-constrained environments. By reducing the incidence of unnecessary tests and treatments through precise diagnostics, it lowers the financial burden on healthcare systems and patients alike. This affordability aligns with global health initiatives aimed at ensuring equitable access to cutting-edge medical tools, regardless of geographic or socioeconomic barriers. As a result, the technology holds the promise of transforming prostate cancer outcomes on a worldwide scale, supporting efforts to create a more inclusive healthcare landscape where advanced screening is not a privilege but a universal standard.
Paving the Way for Future Innovations
Reflecting on the strides made by this AI-powered MRI system, it’s evident that a significant milestone has been reached in the realm of medical diagnostics. Its successful validation and integration into clinical practice demonstrate that artificial intelligence can address longstanding challenges in prostate cancer detection with unmatched precision and reliability. The system’s ability to standardize outcomes, enhance efficiency, and uphold ethical standards sets a powerful example for how technology can complement human expertise in healthcare. Moreover, its impact on reducing global health disparities underscores the potential for innovation to create meaningful social change, ensuring that advanced care reaches those who need it most.
Looking ahead, the groundwork laid by this advancement invites exploration into broader applications and continuous improvement. Stakeholders in healthcare and technology are encouraged to invest in further research, expanding the system’s capabilities to other forms of cancer and integrating additional data sources for personalized medicine. Collaboration between clinicians, policymakers, and technologists will be essential to scale this innovation responsibly, addressing regulatory and practical challenges. By fostering such partnerships, the medical community can build on this success, driving forward a future where AI continues to transform diagnostics, ultimately improving patient outcomes across diverse populations and settings.