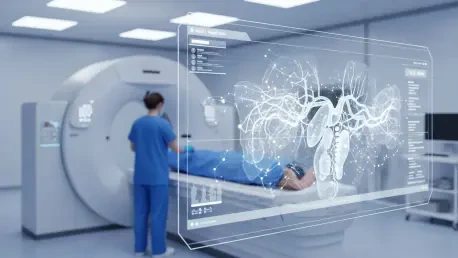
The human eye, trained by years of rigorous medical education and practice, has long been the gold standard in interpreting the complex grayscale landscapes of medical imaging. Yet, the sheer volume of scans and the subtle nature of some pathologies present an ongoing challenge, where even the most experienced radiologist can face uncertainty. Recent advancements in artificial intelligence are beginning to reshape this reality, not by aiming to replace clinical experts, but by equipping them with a powerful digital collaborator capable of perceiving patterns and changes that might otherwise elude human detection. The integration of deep clinical AI platforms is demonstrating a significant capacity to enhance diagnostic performance, streamline workflows, and deliver measurable economic value to healthcare systems. As highlighted by a wealth of scientific abstracts presented at the 2026 International Stroke Conference, these FDA-cleared solutions are proving to be more than just theoretical concepts; they are becoming indispensable tools in modern medicine, particularly in high-stakes fields like neurology and emergency care.
Enhancing Diagnostic Precision
The primary value proposition of AI in radiology lies in its ability to augment human perception, leading to more accurate and timely diagnoses. By processing vast datasets with unparalleled consistency, these algorithms can identify minute anomalies and track their progression over time with a level of objectivity that complements the nuanced, contextual understanding of a human expert. This synergy between machine and clinician is elevating the standard of care, particularly in detecting life-threatening conditions where early and accurate identification is paramount. The technology serves as a vigilant partner, flagging potential areas of concern and providing quantitative data that supports more confident and informed decision-making, ultimately translating into improved patient outcomes.
Aneurysm Growth Detection
One of the most compelling applications of this technology is in the longitudinal monitoring of cerebral aneurysms, where the risk of rupture is directly linked to changes in size and shape. A landmark study demonstrated the superior capability of an AI platform in this domain, revealing that it identified 46% more instances of clinically significant aneurysm growth when compared to the interpretations of neuroradiologists alone. In the analysis, the AI system successfully detected 27 out of 28 documented growth events, whereas human experts identified only 14 of those same events without assistance. This stark difference underscores the challenge of visually comparing scans taken months or even years apart and spotting subtle morphological changes. The AI’s success stems from its ability to perform precise, pixel-by-pixel comparisons, removing the subjectivity inherent in manual assessment and providing a consistent, reliable method for tracking aneurysm progression, which is critical for timing preventative interventions and saving lives.
This advanced capability transforms aneurysm surveillance from a qualitative art into a quantitative science, providing a robust safety net that minimizes the potential for human oversight. The AI platform functions as an ever-watchful second reader, meticulously analyzing each new scan against its predecessors to flag even the slightest variations that could signal an increased risk of rupture. For clinicians, this provides an unparalleled level of confidence in their assessments, allowing them to manage patients more proactively. Instead of relying solely on visual memory or manual measurements, they are equipped with objective, data-driven evidence of an aneurysm’s stability or growth. This enhanced precision is not about second-guessing the radiologist but about empowering them with a tool that can tirelessly perform a task that is both cognitively demanding and critically important. The result is a more standardized, reliable, and ultimately safer approach to managing a condition where the margin for error is virtually nonexistent.
Acute Stroke Diagnosis
In the high-pressure environment of acute stroke care, where every second directly impacts a patient’s prognosis, the speed and accuracy of diagnosis are of the essence. Research into Lumina 3D, an automated three-dimensional reconstruction solution, has shown its profound value in this critical setting. A multi-reader study revealed that incorporating this AI tool improved diagnostic accuracy for detecting stroke-related vessel occlusions and stenoses from 76.1% to a more robust 85.6%. Beyond this significant boost in precision, the technology also streamlined the interpretation process, reducing the time required by an average of 34 seconds per case. For general radiologists, who may not have the same level of specialized neuroradiology training, the time savings were even more substantial, often exceeding one minute per scan. In a field governed by the principle that “time is brain,” these efficiencies are not merely incremental; they are potentially life-altering, enabling clinical teams to initiate crucial treatments faster and improve the chances of a positive outcome.
The operational advantages of automated 3D reconstruction extend deep into the clinical workflow, revolutionizing a process that was once a manual and time-consuming bottleneck. Traditionally, a skilled technologist would need to spend considerable time at a console meticulously building these complex vascular maps from raw scan data. The Lumina 3D solution automates this entire procedure, producing high-quality, standardized visualizations almost instantaneously. This ensures that every clinician, from the emergency physician to the consulting neurologist, receives an optimal and consistent view of the patient’s vasculature, facilitating faster and more accurate decision-making. By removing the manual step, the technology not only accelerates the time to diagnosis but also frees up technologists to focus on patient care and safety. This seamless integration of AI-driven automation helps create a more efficient, responsive, and effective stroke care pathway from the moment a patient arrives in the emergency department.
Streamlining Radiology Operations
Beyond its direct clinical impact on diagnosis, AI is proving to be a transformative force in optimizing the operational efficiency of radiology departments. As healthcare systems grapple with rising costs, staffing shortages, and an ever-increasing demand for imaging services, technologies that can automate routine tasks and maximize resource utilization are becoming essential. AI-powered platforms are addressing these challenges head-on by reducing the manual workload on technical staff, accelerating patient throughput, and creating new avenues for revenue generation. This operational enhancement ensures that the clinical benefits of advanced imaging are delivered in a sustainable and economically viable manner, strengthening the entire healthcare ecosystem.
Alleviating Technologist Workload
A nationwide shortage of computed tomography (CT) technologists has placed immense strain on imaging departments, making workflow efficiency a paramount concern. An assessment of Lumina 3D’s operational impact highlighted its ability to directly address this issue by automating the labor-intensive process of image reconstruction. The study found that implementing the solution reduced the time technologists spent on this task by a staggering 77.4%, slashing the average time per patient from 31 minutes down to just seven. This 24-minute saving per scan is a significant operational gain, freeing up highly skilled technologists from tedious, repetitive work at a computer console. By offloading this burden, the AI allows these critical staff members to dedicate more time to direct patient care, such as positioning, safety checks, and managing the flow of examinations. This not only enhances departmental throughput but also improves job satisfaction and helps mitigate the risk of burnout among essential personnel.
The benefits of this reclaimed time cascade throughout the entire imaging department and beyond, fostering a more agile and patient-centric environment. The 24-minute reduction per scan translates into faster overall turnaround times for diagnostic reports, which in turn reduces patient anxiety and allows referring physicians to make treatment decisions more promptly. For the department itself, this newfound efficiency means a greater capacity to handle both scheduled and emergency cases, helping to clear backlogs and improve access to care. Furthermore, by allowing technologists to step away from the console, the technology empowers them to focus on higher-value activities that directly impact quality and safety. They can provide better patient support, double-check protocols, and ensure the imaging process is as smooth and effective as possible, elevating the standard of care while simultaneously optimizing operational performance.
Generating Tangible Economic Benefits
The operational efficiencies delivered by AI automation translate directly into substantial and measurable economic advantages for healthcare institutions. The study analyzing the impact of automated 3D reconstruction quantified these benefits with striking clarity. The 24 minutes saved per scan aggregated to an estimated 81.6 hours of technologist time saved each month. This newly available capacity enabled the facility to perform an additional 108 scans monthly, generating approximately $43,000 in extra imaging revenue during that period. Such figures provide a compelling business case for the adoption of AI, demonstrating a clear and rapid return on investment. In a healthcare landscape characterized by constant pressure to control costs while improving care, solutions that can simultaneously enhance clinical outcomes, boost operational capacity, and create new revenue streams represent a powerful strategic advantage for any medical center.
This financial impact underscores a pivotal shift in how AI is perceived within healthcare administration—from a costly, futuristic technology to a practical, value-generating asset. The ability to perform more scans without needing to invest in additional hardware or hire more staff directly addresses key economic challenges. It allows hospitals to maximize the utilization of their existing high-cost imaging equipment, turning what might have been idle time into a productive, revenue-generating activity. This financial upside, combined with the proven clinical and operational benefits, completes the value proposition of AI in radiology. It illustrates that investing in intelligent automation is not merely an expense but a strategic decision that strengthens the financial health of the institution, ensuring its ability to continue providing state-of-the-art care in a sustainable and efficient manner for years to come.
A New Era of Collaborative Intelligence
The integration of artificial intelligence into radiology marked a significant turning point, shifting the paradigm from solitary human interpretation to a synergistic collaboration between clinician and machine. The evidence presented has decisively shown that AI platforms are not merely theoretical novelties but practical tools that deliver enhanced diagnostic accuracy, streamlined operational workflows, and tangible financial returns. By detecting subtle aneurysm growth more reliably than the human eye and by accelerating critical stroke diagnoses, these systems have proven their capacity to augment clinical expertise and directly improve patient outcomes. The profound impact on departmental efficiency, particularly in alleviating the workload of strained technologists and creating substantial new revenue, further solidified the technology’s value proposition. This journey has demonstrated that the future of medical imaging lies not in a contest between human and artificial intelligence, but in their powerful, combined potential to elevate the standard of care.