Imagine a world where chronic conditions like inflammatory bowel disease (IBD), affecting millions globally, could be managed without the devastating side effects of current treatments, offering hope to those who suffer daily. For patients with Crohn’s disease, infections caused by an invasive strain of Escherichia coli (E. coli) often worsen their condition, as this harmful gut bacterium resists multiple antibiotics and inflames the intestines. Traditional broad-spectrum antibiotics, while sometimes effective, wreak havoc on the delicate balance of the gut microbiome by killing off beneficial bacteria alongside the harmful ones. Now, a groundbreaking development in drug discovery, powered by artificial intelligence (AI), offers a glimmer of hope. A new antibiotic called enterololin, specifically designed to target this invasive E. coli strain, promises a precision approach that could revolutionize treatment for IBD patients. This advancement highlights the potential of technology to address long-standing medical challenges with unprecedented accuracy.
Revolutionizing Antibiotic Development with AI
Harnessing Machine Learning for Precision Drugs
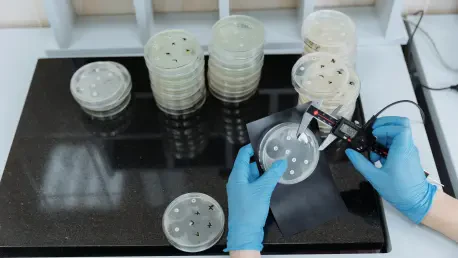
The journey to create enterololin represents a significant leap forward in how antibiotics are developed, moving away from the lengthy trial-and-error methods of the past. Spearheaded by a team at McMaster University in Canada under Jonathan Stokes, this project utilized a machine learning (ML) diffusion model to screen over 10,000 molecules, pinpointing those most effective against the resistant E. coli strain linked to IBD. What sets enterololin apart is its structural uniqueness compared to existing antibiotics, a trait uncovered through a blend of computational predictions and experimental validation. The AI not only identified the compound but also predicted its mechanism of action (MOA), targeting a protein complex responsible for antibiotic resistance in the Enterobacteriaceae family. Remarkably, this process took just six months and cost $60,000, a stark contrast to the traditional timeline of two years and expenditure of around $1 million. This efficiency underscores the transformative power of AI in accelerating drug discovery for urgent medical needs.
Impact on Speed and Cost of Drug Discovery
Beyond the creation of enterololin, the broader implications of AI in drug development are becoming increasingly evident as the technology reshapes the pharmaceutical landscape. The ability to sift through vast chemical libraries and predict effective compounds slashes both time and financial barriers that have historically hindered innovation in antibiotics. In the case of enterololin, pairing it with SPR741—a compound that weakens the outer membrane of Gram-negative bacteria—resulted in a minimum inhibitory concentration (MIC) of just 30 ng/ml, far below the typical 1 µg/ml of many antibiotics. This potency was demonstrated in mouse models, where the combination eradicated invasive E. coli with minimal disruption to beneficial gut microbes, even at high doses. Such precision offers a glimpse into a future where AI-driven solutions could tackle multidrug-resistant bacteria more effectively, addressing a critical global health challenge with cost-effective and rapid results that were previously unimaginable.
Potential and Challenges in Treating Gut Infections
Promising Results for IBD Patients
For the 30% of IBD patients grappling with infections from invasive E. coli, the development of enterololin could mark a turning point in managing their condition with reduced collateral damage. Unlike broad-spectrum antibiotics that indiscriminately eliminate both harmful and helpful bacteria, this AI-designed drug focuses narrowly on the problematic strain, preserving the gut’s anti-inflammatory microbiota. In preclinical studies, the combination of enterololin and SPR741 showed no adverse effects in mouse models, successfully clearing the harmful bacteria from intestinal contents. Experts like Olivier Espéli, a bacteriologist from Collège de France, have hailed this approach as particularly exciting, noting that maintaining beneficial microbes could break the destructive cycle of inflammation in Crohn’s disease. This targeted therapy aligns with a growing demand for treatments that prioritize the delicate balance of the gut microbiome while addressing specific pathogens.
Hurdles in Translating Lab Success to Clinical Use
Despite the optimism surrounding enterololin, significant challenges remain before it can become a viable treatment for human patients suffering from gut infections. A key concern, raised by gastroenterologist Maria Teresa Abreu from Cedars-Sinai Hospital, centers on the limitations of the mouse models used in testing. While the studies effectively cleared E. coli from luminal contents, they did not address the bacteria’s intracellular presence within macrophages—a critical factor in its pathogenicity for IBD. Human trials are essential to confirm the drug’s clinical relevance and effectiveness against these hidden infections. Moreover, no AI-designed antimicrobial has yet successfully passed human testing, casting a shadow of uncertainty over the scalability and real-world impact of such innovations. This cautious outlook emphasizes the need for rigorous follow-up studies to bridge the gap between promising lab results and tangible benefits for patients.
Future Directions for Research and Testing
Looking ahead, the path forward for enterololin and similar AI-driven drugs involves a concerted effort to address unresolved questions and validate their efficacy in diverse settings. The next critical step lies in designing and conducting human clinical trials to assess how well the drug performs against intracellular E. coli infections and whether it can maintain its minimal impact on beneficial gut bacteria in a more complex human environment. Additionally, researchers must explore potential resistance mechanisms that the targeted bacteria might develop over time, ensuring the long-term viability of this treatment. Collaboration between AI specialists, microbiologists, and clinical experts will be vital to refine these therapies and adapt them to the nuances of human physiology. As this field evolves, the insights gained from enterololin’s development could pave the way for a new era of personalized antibiotics tailored to specific infections and patient needs.